Arrhythmias represent a significant clinical concern for patients, often presenting with pronounced symptoms and potentially adverse prognoses. They are disorders of the normal heart rhythm, which is normally regulated by a specialized pacemaker located within the heart, the sinoatrial (SA) node.
Under normal conditions, the heart-which consists of four chambers: two atria (right and left) at the top and two ventricles (right and left) at the bottom-functions through an electrical impulse generated by the SA node in the right atrium. This impulse is transmitted through a specialized conduction system, including the atrioventricular (AV) node, His bundle, right and left bundle branches, and Purkinje fibers, reaching all areas of the heart.
Any disruption in the generation or conduction of this electrical signal can lead to arrhythmias, which may manifest as palpitations or a fluttering sensation in the chest, or in more severe cases, as syncope (loss of consciousness), potentially resulting in sudden cardiac death. Broadly speaking, arrhythmias are classified into bradycardias (slow heart rhythms) and tachycardias (fast heart rhythms).
Types of Bradycardia
- Sick Sinus Syndrome: Impaired generation of the electrical impulse by the sinoatrial (SA) node.
- Atrioventricular (AV) Block: Impaired conduction of the electrical impulse at any point along the specialized conduction system
- Tachy-Brady Syndrome: Alternating periods of rapid and slow heart rates
Types of Tachycardia: Classified according to the site of origin: supraventricular tachycardia and ventricular tachycardia.
A. Supraventricular Tachycardias
Atrial fibrillation: the most common arrhythmia in adults, with increasing prevalence as age rises. It is a chaotic, rapid rhythm, usually originating from the left atrium, specifically at the ostia of the pulmonary veins. Depending on the duration of occurrence, it is classified as: paroxysmal, persistent, and permanent atrial fibrillation. It is associated with an increased number of cerebrovascular events, heart failure, cardiac mortality, and poor quality of life.
Atrial flutter: a similar arrhythmia to atrial fibrillation, with the difference that it often exhibits regularity. In approximately 30% of cases, it coexists with atrial fibrillation in the same patient.

Atrioventricular tachycardia with reentry in the AV node, Atrial tachycardia
Reentrant tachycardia: caused by a reentry circuit located at the atrial-ventricular boundaries. It is triggered by a second conduction pathway (accessory pathway) that, when combined with the normal conduction pathway, creates a closed-loop circuit, leading the heart to beat very fast and rhythmically. In the vast majority of cases, it is not life-threatening, but it significantly affects the patient’s daily life.
B. Ventricular Tachycardias
Originating from the ventricles, these represent the most concerning type of tachycardia, as they can be life-threatening, especially when associated with underlying heart disease.
Common causes of these arrhythmic conditions include:
- Calcification of the conduction system due to advanced age,
- Coronary artery disease,
- Structural heart diseases,
- Electrolyte imbalances,
- Medication effects.
Symptoms: a fluttering sensation in the chest, which may be accompanied by pain, dizziness, fainting, shortness of breath, easy fatigue, and weakness.
Diagnosis of Cardiac Arrhythmias
12-lead Electrocardiogram (ECG): captures the heart’s rhythm and the speed at which it beats.
Ambulatory rhythm monitoring (Holter monitor): used when the ECG appears normal but suspicion for an abnormal rhythm remains.
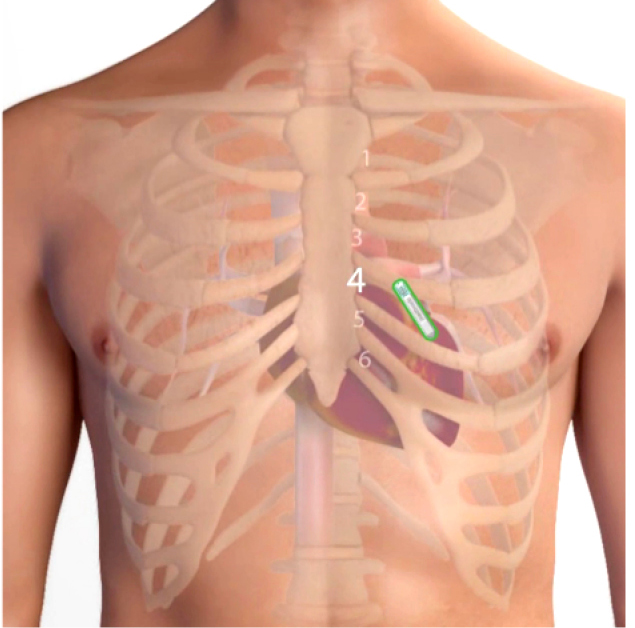
Implantable Rhythm Recorder
Implantable Rhythm Recorder: used when arrhythmias occur at long intervals, typically greater than one month. This is a very small device, approximately 1.2 cc in volume, implanted in a brief procedure (1–2 minutes) to the left of the sternum, without requiring patient hospitalization.
Exercise Stress Test: Helps detect arrhythmias, especially those triggered by physical exertion.
Cardiac Triplex: Provides information on valve function and the heart’s pumping efficiency.
Tilt Table Test: Performed in patients with syncope when malignant parasympathetic activity is suspected.
Cardiac MRI: Offers detailed information on heart function and structural composition.
Electrophysiological Study (EPS): An invasive test performed via catheters inserted through the femoral vein into the heart, indicated when prior non-invasive tests fail to diagnose the arrhythmia.
Coronary Angiography: Performed if there is strong suspicion of coronary artery disease based on previous tests or patient symptoms.
Management of Bradycardias: Bradycardia is often caused by medications used for other conditions or by underlying disorders (e.g., hypothyroidism). In such cases, adjusting medications or treating the underlying condition can resolve the problem. Otherwise, permanent implantation of a pacemaker-a device generating electrical pulses-restores a sufficient heart rate (typically above 60 bpm), ensuring the body’s circulatory needs are met.
Pacemaker Types
Transvenous Pacemaker:
Consists of a generator implanted under the skin, approximately 2 cm below the clavicle, connected to leads (1 or 2 depending on the patient’s underlying rhythm) that pass through the venous system into the heart. This has been the most effective and safest treatment for bradycardia for decades.
Biventricular Pacemaker: The main difference from the standard transvenous pacemaker is the presence of a third lead. This additional lead improves synchronization of the heart walls, optimizing cardiac function. It is indicated for patients with moderate to severe heart failure.

Leadless Pacemaker
Leadless Pacemaker: This represents the latest technological advancement, combining the generator and leads into a single, very small device (less than 1 cc). The device, mounted on a catheter, is delivered percutaneously through the femoral vein and implanted directly into the heart. It is highly effective, safe, and patient-friendly, offering a discreet solution without a scar in the subclavian area, as the pacemaker is not visible externally.
Management of Tachycardias
Antiarrhythmic Drugs: These are medications that act at the cellular level on cardiac cells to reduce or prevent the occurrence of tachycardias. Their effectiveness varies depending on the type of tachycardia, and in some cases, they may cause significant side effects.
Interventional Ablation Therapy: This is the treatment of choice for most types of tachycardias. It offers superior efficacy compared to medication, often providing a permanent solution for many of the tachycardias mentioned earlier. Advances in technology over the past decade have made this procedure highly safe. It is performed percutaneously via the femoral veins or arteries, similar to an electrophysiological study. The difference lies in the ablation catheter, which delivers thermal energy to the heart’s internal wall, causing controlled destruction of the targeted tissue.
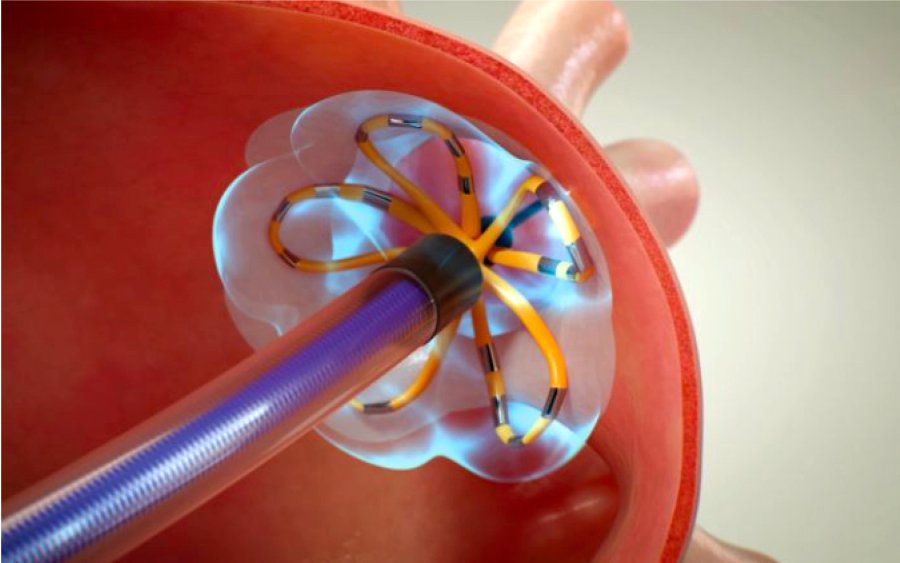
Atrial Fibrillation Ablation Using Pulsed Field Ablation
Specifically for atrial fibrillation, beyond the established ablation techniques using three-dimensional mapping with radiofrequency energy or balloon-based cryoablation, a new energy source—Pulsed Field Ablation (PFA)—has been increasingly used in recent years. This method offers high safety, effectiveness, and reduced procedure time. Its main advantage lies in its ability to selectively destroy pathological myocardial cells while leaving the surrounding tissues intact.
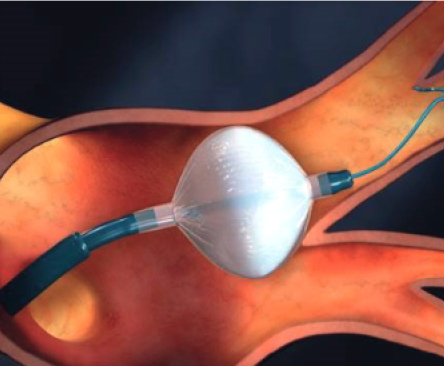
Atrial Fibrillation Ablation Using Balloon Cryoablation
Implantable Transvenous Defibrillators (ICDs): These devices represent the cutting edge of therapy for patients with heart failure who are prone to ventricular tachycardias. Essentially, they function as pacemakers but also have the capability to deliver stored electrical energy directly to the heart (defibrillation), interrupting ventricular tachycardia and restoring normal rhythm. The use of ICDs has dramatically improved survival outcomes in patients with heart failure.
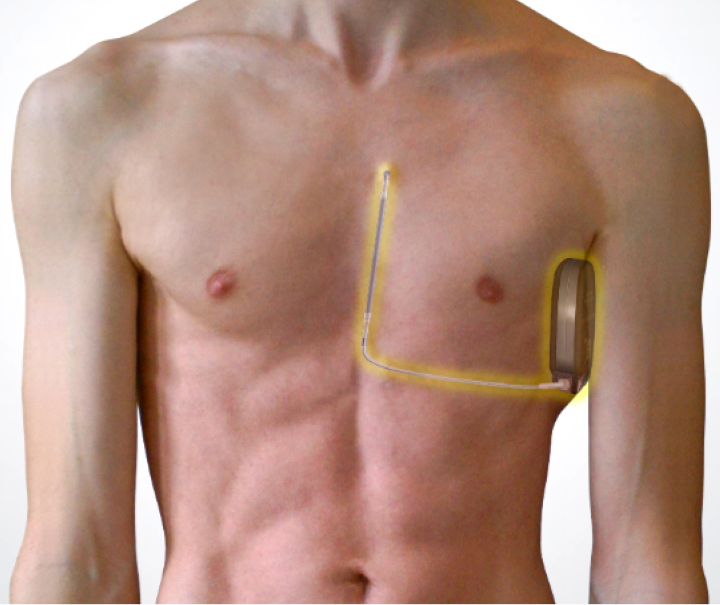
Subcutaneous Defibrillator
Subcutaneous defibrillators have made a significant contribution for patients with ventricular tachycardias, offering the advantage of avoiding the use of the venous system for defibrillator lead implantation.
In this context, the Electrophysiology and Pacing Department at Metropolitan Hospital integrates all modern methods and techniques to provide medical services at the highest level, based on three pillars: timely diagnosis, appropriate treatment, and systematic follow-up of patients with arrhythmias. With its specialized team, the department performs a large number of ablation procedures for all types of tachycardias annually, achieving high success and safety rates. It is also a recognized center for the implantation of pacemakers, defibrillators, and biventricular cardiac resynchronization systems.