Our thirty years of experience and strong presence in top-level Greek microsurgery practices have led to the establishment of the Metropolitan Hospital Upper Limb Surgery and Reconstructive Microsurgery Team.
This team aims to provide the most comprehensive and timely treatment of upper limb and peripheral nerve injuries and conditions, using traditional and innovative surgical techniques, while at the same time showing kindness and compassion towards patients and working closely with other health professionals.
The Department accepts emergencies 24/7, all year round.
Detection and repair of very small anatomical structures of the body
The term "microsurgery" refers to the surgical technique that uses a surgical microscope.
This technique permits the detection and repair of very small anatomical structures of the body, such as anastomosis of very small vessels and nerves (typically around 1mm in diameter), transfer of tissue from one part of the body to another, and replantation of amputated limb parts.
Upper limb surgery deals with the surgical and conservative treatment of all hand and upper limb conditions. These conditions prevent the patient from performing various operations necessary for daily activities.

The Metropolitan Hospital Microsurgery Department specializes in the following conditions:
- Brachial plexus surgery
- Peripheral nerve surgery
- Congenital disorders
- Vascularized tissue transfer
- Skin defect coverage
- Hand surgery (skin, bones, joints, tendons)
- Obstetrical paralysis
Brachial Plexus Surgery
The brachial plexus is a complex nervous formation with the nerve stems originating from the spinal cord and providing motor and sensory function to the entire upper limb.
Adult brachial plexus palsy is mainly caused by traffic accidents, with the vast majority of cases (90%) being caused by motorcycle falls.
This avulsion injury can affect some or all of the stems, with a similar impact on upper limb function.
Microsurgical repair involves restoration of the continuity of the nerve stems using nerve grafts or nerve transfer in avulsion injuries (cerebral conjunctions, intercostal nerves) and their connection with the peripheral motor branches.
Patient hospitalization time is 3-4 days, followed by physiotherapy regimen after the 3rd week.
Patients are monitored systematically in outpatient clinics and reassessed at regular intervals.
Overall during the last 25 years, more than 400 cases of traumatic brachial plexus damage have been treated.
With accumulated clinical experience of 25 years, one of the largest clinics is being established within the EU. The clinic results and conclusions have been presented in Greek and international medical conferences.
Peripheral Nerve Injuries
Upper and lower extremity peripheral nerve injuries are of varying size and severity and have a major impact on motor and sensory function. They are usually accompanied by injuries in other tissues, such as bone, muscle, tendons and skin.
They are usually caused by:
- Injuries from cutting instruments
- Car accidents
- Work accidents
- Nerve tumor removal surgery
- Iatrogenic injury during surgery
Surgical investigation of such injuries using a surgical microscope reveals the extent of damage and leads to a decision about immediate or subsequent microsurgery repair, minimizing the complications and optimizing the results.
The decision must be made after taking into account the total damage and requires extensive experience in peripheral nerve surgery, in order to expect satisfactory motor and sensory function.
Newer techniques such as endoscopic carpal tunnel surgery, neurotransmission, use of nerve conductors and allografts are appropriately used and indicated by experienced microsurgeons.
Special tendon transmission and neurotransmission techniques can help paralytic hand or foot function, even in patients with quadriplegia.
Total Skin Thickness Deficits / Vascularized Skin Graft Transfer
In extensive total skin thickness deficits, coverage is achieved by selected skin flaps, based on arterial stems, which provide functional coverage of deficits, following microsurgical anastomosis with the vessels of the receiving area.
Except for the primary purpose of covering the deficit, this method provides blood flow to the injury site, resulting in better healing of the related lesions (in bones, tendons, nerves) and the possibility of reconstructive interventions at a later date.
Toe-to-hand Transfer
This method is based on the particular autonomous perfusion of toes and applies to cases of reconstruction of an amputated thumb or in cases of loss of more than two fingers.
Congenital Dysplasias Of The Upper Limb
The clinical condition of congenital anomalies of the hand is classified in failure of formation or separation (syndactylies).
In each case, and depending on the condition, surgical treatment aims to restore the function of the hand and improve the aesthetic result.
Upper Limb Fractures
The introduction of minimally invasive techniques and new materials has changed the state of affairs in shoulder, elbow and hand fracture treatment.
Fractures such as those in the region of the distal radius and navicular, as well as heavier injuries in the region of the elbow and shoulder, can now be treated with surgery through small incisions, allowing quicker mobility restoration, limiting immobilization ankylosis, and at the same time enabling patients to return to work and their social life faster.
Wrist, Elbow And Shoulder Arthroscopy
The use of a small camera and special tools revolutionized knee and shoulder surgery, making it possible to perform major procedures through small holes.
Even smaller cameras and tools now permit surgeons to also operate on the elbow, wrist and finger joints using the same method. The Metropolitan Hospital Microsurgery & Upper Limb Surgery is a pioneer in these techniques.
Upper Limb Arthroplasty
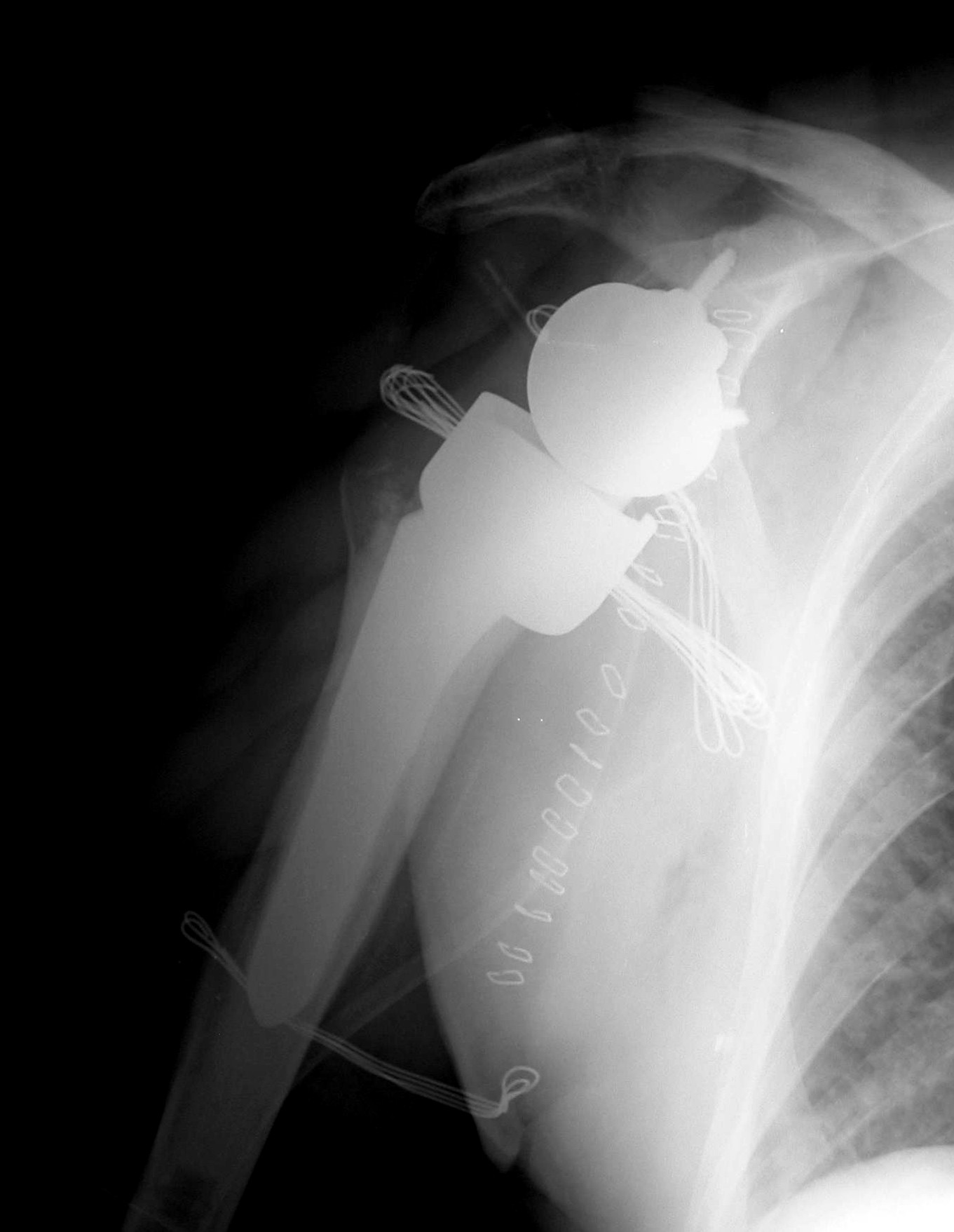
Continuing its successful tradition in knee and hip arthroplasty, replacements are also performed for shoulder, elbow, wrist and fingers in advanced arthritis (post traumatic, degenerative, rheumatoid).
At the same time arthroplasty without extraneous materials (inserting patient tendons or fascia) is possible, especially in arthritis of the thumb base and small joints of the hand, as well as the elbow and shoulder in selected patients.